Brachytherapy is an integral part of the management of cervical cancer for cases where radiation therapy is the primary treatment.
Cervical cancer is one of the most preventable and treatable types of gynecological cancers worldwide. According to current data, cervical cancer is the 4th most common cancer among women globally.
The cervix is the lower part of the uterus that connects the vagina (birth canal) and the uterus. Cervical cancer occurs when normal cells of the cervix undergo DNA mutations and begin to grow out of control.
Over time, the abnormal cells may become invasive cancers that can spread to other parts of the body and can be fatal. Most cervical cancers are caused by a previous infection with human papillomavirus (HPV) spread during vaginal, anal, or oral sex.
Like most cancers, cervical cancers can be managed effectively when diagnosed early.
What is Brachytherapy?
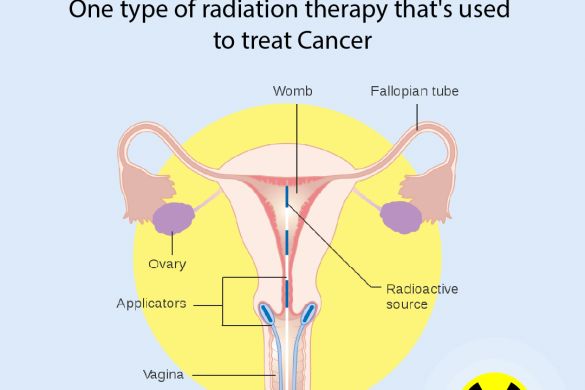
Brachytherapy, or internal radiation therapy, is a type of radiation therapy in which a device (catheter or implant) is placed inside the patient to deliver radioactive material directly to cancer cells.
This allows high doses of radiation to be delivered precisely to targeted areas to kill cancer cells or prevent their growth.
Brachytherapy is often used to treat cancers of the head and neck, breast, cervix, prostate, eye, and soft tissue sarcomas.
The type used for cervical cancer is known as intracavitary brachytherapy, where the radiation source is placed inside the vagina or cervix near the tumor to deliver a high total dose in less time.
Why is Brachytherapy Done?
According to the International Federation of Gynecology and Obstetrics (FIGO), all women with locally advanced cervical cancer (stage IB2–IVA) should be considered for brachytherapy as part of their main treatment.
For advanced-stage cancers, it is performed after external radiation therapy to improve treatment outcomes.
Compared to other radiation methods, brachytherapy delivers a curative dose precisely to the target cells, reducing damage to surrounding organs like the rectum, bowel, and bladder.
What Are the Different Types of Brachytherapy?
Temporary Brachytherapy
The radioactive material is inserted and removed at the end of each session.
Low-Dose Rate (LDR)
Delivers radiation continuously at a low dose over several days. The patient is isolated in a shielded room during treatment. This method is now obsolete.
High-Dose Rate (HDR)
The radioactive material is inserted for a few minutes and then removed. Each session lasts 10–20 minutes.
HDR is usually an outpatient procedure but may require short hospitalization depending on the patient's condition.
Performed under general anesthesia or moderate sedation. The entire process typically takes 2–3 hours per session.
Permanent Brachytherapy
Involves implanting radioactive seeds next to the tumor. The seeds remain in the body permanently, but radiation diminishes over time.
This method is rarely used for cervical cancer.
What Are the Risks?
Brachytherapy mainly affects the cervix and vaginal walls. Side effects include:
Short-Term Side Effects
- Sore vagina
- Mild vaginal bleeding or discharge
- Irritation of vulva and vagina
- Fatigue
- Diarrhea
- Nausea
- Burning sensation when urinating (similar to cystitis)
- Deep vein thrombosis (DVT)
Long-Term Side Effects
- Vaginal stenosis (narrowing and shortening of the vagina)
- Vaginal dryness
- Weakened bones
- Swelling of the leg(s)
- Early menopause and infertility
- Rectal bleeding or rectal stenosis
How to Prepare for the Procedure?
Pre-surgical testing includes reviewing medical history and performing blood and imaging tests to finalize anesthesia type.
You may receive instructions such as:
- Temporarily discontinue medications like aspirin or ibuprofen
- Stop smoking and drinking to aid recovery
- Follow a clear liquid diet the day before
- Do not eat or drink after midnight before the procedure
What to Expect During the Procedure?
- Hospitalization may be needed a day before or after.
- After anesthesia, you’ll be positioned comfortably.
- A vaginal exam determines the size of applicators based on anatomy and disease extent.
The placement of radioactive material depends on your condition:
- After hysterectomy: Material placed in the vagina using a tube applicator.
- With uterus intact: Material placed in a tandem (metal tube in the uterus) with ovoids or a ring near the cervix.
Cotton gauze packs around the applicators help reduce radiation exposure to the rectum and bladder.
Imaging (MRI preferred, or CT/X-ray) is done after placement to confirm positioning and aid treatment planning.
The applicator is connected to a machine that delivers the planned radiation dose.
Outcome of Brachytherapy
Scanning tests are recommended 6–8 weeks after treatment to assess success.
Brachytherapy is one of the most effective cancer treatments due to its precision and high success rate.
Early-stage patients often get cured with brachytherapy. For later stages, it's combined with other treatments and is most effective when delivered on schedule and in correct doses.
