What Are The Treatment Options for Liver Cancer?
Explore the various treatment options for liver cancer, including surgery, transplantation, ablation, and systemic therapy, based on cancer stage and health.
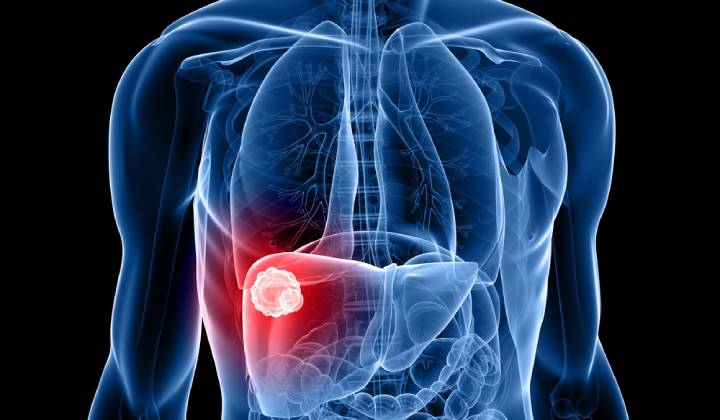
The liver — the body’s largest internal organ — is essential for detoxification and waste elimination, and it is also vulnerable to cancer, both primary (originating in the liver) and secondary (metastatic). Primary liver cancer is most commonly Hepatocellular carcinoma (HCC), which begins in hepatocytes (the main liver cells). Secondary liver cancers are identified by the type of cancer that has metastasised to the liver. Globally, liver cancer is the 5th most common cancer in men and the 9th in women, and incidence is higher in regions such as South East Asia and sub‐Saharan Africa compared with countries such as the US.
Once a diagnosis of liver cancer is made, a multidisciplinary care team determines the treatment plan. The plan is guided by several key factors:
the percentage of liver involved by tumour,
whether the cancer is localised or has spread (extrahepatic spread or vascular invasion),
the patient’s overall health and fitness, and
the condition of the remaining (“cancer-free”) portion of the liver (for example whether there is underlying cirrhosis or impaired liver function).
Based on disease progression and treatability, liver cancer can be divided into the following broad categories:
Resectable or transplantable (curative intent)
Unresectable (local therapy or non-curative intent)
Advanced cases (metastasis or major vascular involvement)
Treatment options include one or more of the following: surgery (resection), liver transplantation, ablative therapies, embolisation/chemo-/radio-embolisation, radiation therapy, systemic therapy (targeted drugs, immunotherapy), and clinical trial enrolment.
Surgery or Resection: When the tumour is small, localised and the patient has good liver function (and minimal cirrhosis), surgical removal of the affected part of the liver is the preferred curative option. Guidelines indicate that resection is the treatment of choice for solitary tumours in patients with preserved liver function. (Medscape)
Liver Transplantation: For patients who meet specific criteria (e.g., the so-called “Milan criteria” — a single tumour ≤ 5 cm or up to three nodules each ≤ 3 cm, without major vascular invasion or extrahepatic disease), transplantation offers a curative option, especially when the liver function is compromised or resection is not feasible. (Medscape)
Ablation & Local Therapies: For early‐stage tumours in patients who are not candidates for surgery or transplant, local ablative therapies — such as radiofrequency ablation (RFA), microwave ablation (MWA), percutaneous ethanol injection (PEI) — are effective alternatives. Ablation can offer outcomes comparable to resection in selected small tumours. (SpringerLink)
Embolisation / Locoregional Therapy: In cases where the cancer is still within the liver but resection/transplant is not possible, locoregional treatments like Transarterial chemoembolization (TACE) or radioembolisation may be used. These therapies block the tumour’s blood supply or deliver treatment directly to the liver. (PMC)
Radiation Therapy: Radiation, including stereotactic body radiotherapy (SBRT) or internal particle therapies (e.g., Y-90 radioembolisation) may be considered in selected patients as part of non-curative or combined approaches. (Karger Publishers)
Systemic Therapy (Targeted / Immunotherapy): For advanced liver cancer (metastasis, major vascular invasion, or when local therapies are no longer suitable), systemic therapy is indicated. Newer agents, including targeted therapies and immunotherapies (for example combinations involving PD-L1/VEGF inhibitors), have become standard in many settings. (Medscape)
Clinical Trials: Given that treatment options for very advanced liver cancer remain limited, a clinical trial may be recommended, offering access to novel therapies and contributing to future care advances.
Prognosis & Importance of Early Detection: If detected in early stages when curative options (resection, transplant, ablation) are feasible, liver cancer can have a favourable prognosis. But delays in diagnosis or detection at a later stage—when the cancer has spread outside the liver or liver function is poor—significantly worsen outcomes.
Summary of key points to keep in mind:
The patient’s underlying liver health (e.g., cirrhosis) is as important as the tumour characteristics in deciding treatment.
A multidisciplinary team approach is essential (surgeon, hepatologist, oncologist, radiologist, transplant specialist).
The “curative intent” treatments (resection, transplant, ablation) are only appropriate if liver function is sufficient and disease is appropriately staged.
Non-curative therapies aim to prolong survival or improve quality of life, not necessarily achieve cure.
Surveillance (in high-risk patients) is crucial to catch tumours when they are small and treatable.
