Cancer is an unforgiving enemy that is hard to comprehend and difficult to talk about. Cancer can happen at any age, and even to persons who seem healthy.
Fortunately, among all cancers, testicular cancer is an easily treatable and relatively rare neoplasm. While the disease can affect men of all ages, including babies, it is more common among young men aged between 15–34 years.
How Common is Testicular Cancer?
Testicular cancer is extremely uncommon worldwide, accounting for only 1–2 percent of all cancers in men.
While a man’s risk of getting the disease is about 1 in 250, his chance of dying from it is even smaller (1 in 5000), thanks to multimodal treatment approaches.
However, evidence suggests that the incidence of testicular cancer is increasing yearly, particularly in industrialized nations. According to reports, the number of cases has doubled in the last four decades, rising from 3.7 per 100,000 people in 1975 to 6.3 per 100,000 in 2017.
Risk Factors and Demographics
Testicular cancer is more common in certain racial and social groups:
- Men in the United States and Europe are more likely to develop it than men in Asia and Africa.
- White men have a 4–5 times greater risk compared to other ethnicities.
- American Indian men are also at some risk, though lower than white men, and are prone to seminoma cancer.
- Undescended testicle (cryptorchidism) is a major risk factor.
- Family history of testicular cancer increases risk.
- Male infertility is linked to approximately 3 times higher risk.
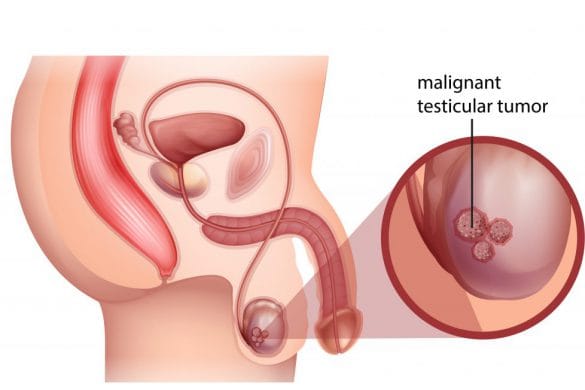
Types of Testicular Cancer
About 95% of testicular cancers are germ cell tumors, categorized into two main subtypes:
- Seminoma: Less aggressive and highly sensitive to radiation and chemotherapy.
- Non-Seminoma: More common in younger men, spreads quickly, and requires aggressive treatment.
A mixed type contains both seminoma and non-seminoma cells and is treated as non-seminoma.
Common Symptoms
- A painless lump or swelling in a testicle
- A feeling of heaviness in the scrotum
- Dull ache in the abdomen or groin
- Sudden collection of fluid in the scrotum
- Pain or discomfort in a testicle or scrotum
- Enlargement or tenderness of breast tissue
Diagnosis and Tumor Markers
Diagnosis involves physical examination, ultrasound, and blood tests for tumor markers:
- Alpha-fetoprotein (AFP) – elevated in non-seminomas
- Beta-hCG – elevated in both types
- LDH – general marker of tumor burden
Note: Results may show "false positives," so other tests are needed to confirm cancer.
Treatment Approach
The first line of treatment for suspected testicular tumors is radical inguinal orchiectomy — surgical removal of the affected testicle through an incision in the groin (not the scrotum).
Further treatment depends on the type and stage:
- Seminomas: Often treated with radiation or chemotherapy after surgery.
- Non-Seminomas: May require chemotherapy and retroperitoneal lymph node dissection (RPLND).
Prognosis and Survival
Testicular cancer is largely treatable. The five-year survival rate exceeds 95% when caught early. Even in advanced stages, cure rates remain high due to sensitivity to chemotherapy.
Regular self-exams and prompt medical attention for any abnormalities are crucial for early detection.
